Some ingredients are everywhere, essential parts of our favourite dishes and indulgences. What is tolerable for some may be intolerable for others. Food intolerances are common, and much more so than many people believe. Intolerances are often underlying conditions that can cause mysterious symptoms. That makes testing for gluten intolerance and other intolerances a good idea if you are living with strange symptoms. Especially if you are looking for relief! Below, we’ll explain more about gluten intolerance and the most common gluten intolerance symptoms. This information can help you to decide what next step is best for you.
What exactly is gluten intolerance?
If you are gluten intolerant, your body is physically unable to digest the active protein in gluten, called gliadin. It is safe to eat gluten-containing foods, but not recommended. After all, the body will struggle to digest them. Gluten intolerance symptoms can be mild to severe, depending on the intolerance severity.
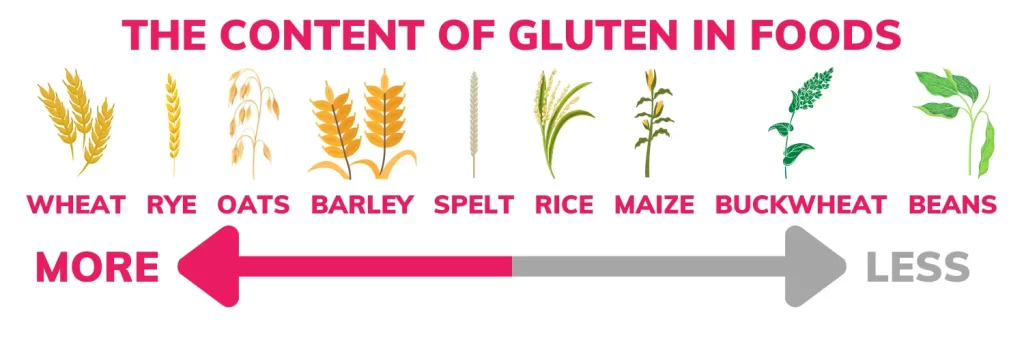
Gluten is in many different foods, and it can feel like a minefield trying to figure out what is okay to eat and what isn’t. The good news is that gluten intolerance is common. So, there are many resources online to help guide your diet and meal plans.
Is gluten intolerance the same as Coeliac disease?
While they sound the same, gluten intolerance is not the same as Coeliac disease. Those living with Coeliac disease can damage their intestines if they eat gluten. It is a dangerous food ingredient for them. If you are gluten intolerant, you can have severe symptoms (which we’ll discuss below), but it isn’t dangerous for the body. Someone with gluten intolerance will not have intestinal damage from eating gluten-containing foods, no matter how much they eat.
Of course, determining whether you have Coeliac disease is essential. You need to know what you’re dealing with. You can do that by approaching your GP. Or, consider testing for gluten intolerance at home. This can help you learn about other food intolerances you were unaware of.
Common symptoms of gluten intolerance

There are quite a few common gluten intolerance symptoms that you can watch for, but the most common ones are below:
Stomach pain
One of the most common symptoms of gluten intolerance is stomach pain. It could be a mild ache or a severe pain that may cause you a lot of concern. While unsettling and scary, it’s important to remember that an intolerance can’t hurt you or cause damage. It will pass.
Diarrhoea and constipation
These two symptoms may seem contradictory, and they are, but they’re also both possible with gluten intolerance. Many people living with an intolerance to gluten can have diarrhoea and constipation. This can be mild to severe as well.
Headaches or migraines
Most people wouldn’t connect the dots between a headache or a migraine and gluten intolerance, but there is a strong connection. These headaches are often the aching kind rather than the sharp pain. Some can have full-on migraines due to gluten intolerance.
Chronic fatigue
Most of the general population is tired, but chronic fatigue is entirely different. This crippling, long-term tiredness can be present in your body no matter how much or how long you sleep. This is a gluten intolerance symptom because the body is working hard to digest the “problem” food ingredient and working overtime!
Joint pain and inflammation
The body will become inflamed as it struggles to digest gluten, so those living with gluten intolerance can have sore joints and general inflammation in the body. Some blame this on the weather or overworking the problem joints, but it could be as simple as what you’re eating.
Brain fog
This is one of the easiest gluten intolerance symptoms to overlook. This is like fatigue you might feel, but in the mind. You’ll have difficulty focusing on things you enjoy and often feel mentally aimless as you try to get things done. This is a classic food intolerance symptom.
Intolerances vs allergies
You can have food intolerances and food allergies. Food intolerances are different from allergies, and the main concern is that a food allergy can be dangerous. An intolerance is a form of indigestion; an allergy is an immune system reaction where your body attacks the problem food. You should never knowingly eat something to which you are allergic.
Gluten intolerance vs. wheat allergy
Other than Coeliac disease, the “dangerous” competition to gluten intolerance is a wheat allergy. Mild wheat allergies can be easily confused with intolerances to gluten. This is especially true if there is no family history of allergies. It’s always best to consider testing for gluten intolerance if you aren’t sure. Then you’ll determine if you are allergic to wheat or intolerant to one of its core ingredients, gluten.
If you’ve seen a lot of information about gluten-free cooking online, you can see why now. With it being as common a problem as it is, many are finding symptom relief in gluten-free options. These substitutions allow food to be enjoyable again. Perhaps most importantly, test results can give you an answer to those strange and mysterious symptoms.